Why Eczema and Psoriasis Flare-Ups Can Worsen during Menopause

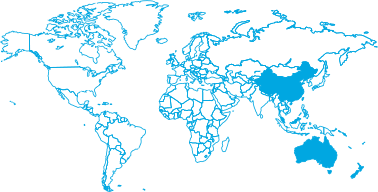
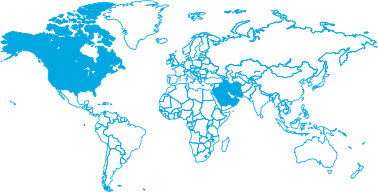
Area
Daily UseKey Takeaways:
- Estrogen is a natural anti-inflammatory: As levels drop during menopause, your skin loses its primary defense against inflammation.
- The barrier becomes “leaky”: Declining hormones reduce lipid and ceramide production, making the skin barrier more vulnerable to irritants that trigger eczema.
- Psoriasis and menopause often peak together: Hormonal changes can activate the immune system, causing a sudden onset or worsening of psoriatic plaques.
- Moisture management is non-negotiable: Using targeted, clinically-tested barrier therapies is the most effective way to support skin recovery during this transition.
Navigating menopause is often described as a “second puberty,” but for many women, the changes aren’t just internal. If you have noticed that your skin is suddenly acting like a stranger, reacting to products you’ve used for years or flaring up with itchy, red patches, you aren’t alone.
This article is part of our comprehensive series, a Guide to Menopause and your Skin, designed to help you reclaim comfort in your skin. While we’ve already explored Why Menopause Causes Dry, Itchy Skin (And What Helps), Sensitive Skin During Menopause: Causes, Triggers and Care Tips, and the Best Skincare Ingredients for Menopausal Skin (And What to Avoid), this guide focuses on the specific relationship between hormonal shifts and chronic inflammatory conditions like eczema and psoriasis.
How do hormonal changes affect existing skin conditions?
Estrogen is the foundational pillar of healthy skin. It supports the production of collagen, hyaluronic acid, and essential lipids (like ceramides) that keep your skin thick, hydrated, and resilient. During menopause, the rapid decline in estrogen leads to significant thinning of the dermis and a decrease in sebum production.
For those with a history of eczema or psoriasis, this means the skin’s “shield” is effectively down. When the skin is thinner and drier, it is more easily penetrated by allergens and environmental triggers. This explains why a mild case of eczema in your 30s can suddenly become an aggressive flare-up in your 50s.
Why does menopause make eczema and psoriasis more aggressive?
It’s not just about dryness; it’s about the immune system. Estrogen typically has a regulatory effect on the body’s inflammatory response. When it disappears, the body can produce an excess of pro-inflammatory cytokines. In psoriasis, these cytokines signal the skin cells to turn over too quickly, leading to the thick, scaly plaques characteristic of the condition.
In eczema, the lack of estrogen leads to a spike in transepidermal water loss (TEWL). As moisture evaporates, the skin becomes “hyper-reactive.” This creates a vicious cycle: the skin itches, you scratch, the barrier is further damaged, and the inflammation worsens. This is often where Dermal Therapy Anti-Itch Soothing Cream can help, as it is tested to soothe that intense “menopausal itch” in minutes.
Can you differentiate between “menopausal dryness” and a clinical flare-up?
It can be tricky. Standard menopausal dryness (xerosis) usually feels like a tight, rough sensation all over. However, if you see distinct, red, inflamed patches that are weeping or intensely itchy, you are likely dealing with menopause eczema. If you notice silver-white scales on red, raised areas, particularly on the elbows, knees, or scalp, it may be hormonal psoriasis.
Because these conditions are inflammatory, they require more than a basic moisturiser. Dermal Therapy Eczema & Dermatitis Cream uses colloidal oatmeal to soothe the barrier, and Dermal Therapy Psoriasis Cream uses urea to soften and remove scales.
How can a targeted skincare routine manage hormonal flare-ups?
Managing menopausal flare-ups requires a “barrier-first” approach. This means replacing exactly what your hormones are no longer providing.
- Switch to a Soap-Free Wash: Traditional soaps strip the few oils your skin has left. Use Dermal Therapy Sensitive Skin Wash to cleanse without disrupting the balance of acids.
- Use Urea-Based Moisturisers: Urea is a gold-standard ingredient for menopausal skin because it is a natural moisturising factor (NMF). Dermal Therapy Very Dry Skin Cream contains 12.5% urea, which is clinically tested to increase skin hydration by 52% in two weeks. Learn more in our Guide to Urea in Skincare.
- Apply to Damp Skin: To lock in maximum moisture, apply your treatments immediately after showering.
Learn more about Eczema here:
- The Ultimate Guide to Face & Eye Eczema
- Eyelid Eczema: Causes and Symptoms
- Ingredients to Use and Avoid Near the Eyes
- How to Manage & Treat Eczema Around the Eyes Safely
References:
- Medicine Today: Skin and hair changes in menopause – it’s not just ageing!
- The American Academy of Dermatology Association – Caring for your skin in menopause
- EAA – Eczema Association of Australasia – Managing Eczema
- National Eczema Association – How Does Menopause Affect Your Eczema?