Eyelid Eczema: Causes and Symptoms

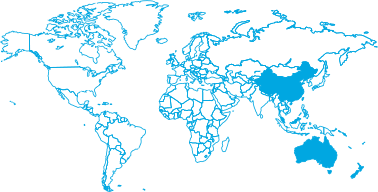
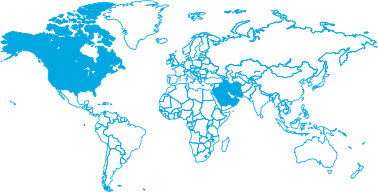
Area
Eczema & DermatitisKey Takeaways:
- The eyelid’s thin skin, dense blood vessels, and rich nerve supply make it highly sensitive and prone to rapid redness, swelling, and intense itching.
- Eyelid eczema is primarily triggered by external factors, as over 60% of referral cases are diagnosed as allergic contact dermatitis from products. 27.5% are linked to atopic eczema, confirming a strong genetic role.
- Lifestyle factors significantly worsen the condition, with surveys reporting that 57% of women and 41% of men cite stress as a key trigger.
If the skin around your eyes is constantly red, swollen, and prone to flaking, you know the frustration that comes with eyelid eczema. It’s more than just dry skin; it’s an inflammatory reaction that leaves you guessing: Is it my makeup, stress, or something else entirely?
This guide provides a clear, science-backed breakdown of the causes and triggers that lead to eczema on the eyelids. We’ll explain how to spot your unique symptoms and identify your triggers to finally find lasting comfort.
What Makes the Eyelids So Sensitive?
The skin on your eyelids is an inflammatory target because it’s hyper-reactive, not just thin.
- The 0.5mm Filter: Eyelid skin is the thinnest on your entire body (0.5 mm). This minimal barrier allows irritants, allergens, and moisture to easily penetrate and escape.
- Rapid Swelling and Redness: The area has a dense network of blood vessels. When exposed to an inflammatory substance, these vessels quickly react and dilate, leading to immediate and noticeable redness and swelling.
- Heightened Itch Response: Eyelids have a high concentration of nerve endings. When stimulated, these nerves converge to aggressively amplify the feeling of itchiness and discomfort.
Because of this unique biology, constant friction and even mild products can quickly trigger a severe reaction, turning a slight irritation into full-blown eyelid eczema.
What Causes Eczema on Eyelids?
The key to managing your flare-ups is stopping the guesswork. So, what causes eczema on eyelids? It comes down to a few core triggers we can help you identify right now.
Allergic Reactions
Eyelid allergies occur when your immune system treats a particular substance as a threat. You need to look for two main types of contact.
- Product Allergens: Common culprits include fragrance (a major sensitiser), nickel (often transferred from eyelash curlers), certain preservatives (MI, MCI), and chemical components in hair dye.
- Airborne & Transfer Allergens: The delicate eyelid skin can be irritated by particles in the air like pollen, dust mites, or pet hair. Pay attention to cross-contamination from hands or nails carrying residue from products like polish or perfume.
Irritant Contact Dermatitis
This type of eyelid dermatitis is not an immune response like an allergy. It occurs when a chemical or physical injury directly damages the skin barrier faster than it can repair itself.
- Harsh Products: Certain ingredients in skincare, strong makeup removers, or irritating chemical sunscreens can chemically strip the protective barrier.
- Physical Stress: Frequent eye rubbing is a common response to itchy eyelids. This causes physical damage and micro-tears in the delicate skin layer.
- Cleaning Agents: Residue from strong hand soaps, cleansers, or hair products can be transferred to the eyes, causing immediate irritation and barrier breakdown.
Atopic Eczema
This type of chronic condition is driven by internal, genetic factors rather than an external irritant. It reflects a lifelong predisposition toward a compromised skin barrier.
- Genetic Link: 39.9% of patients with eyelid eczema report a personal history of atopy (like hay fever or asthma), while 28.9% have a family history, confirming the strong genetic link.
- Skin Barrier Dysfunction: The barrier is genetically faulty, allowing moisture to escape and environmental factors to trigger inflammation more easily.
- Flares Without Obvious Trigger: Because the cause is internal, flare-ups can occur due to factors like illness, or seasonal changes, without clear contact with a new product.
Stress and Lifestyle Factors
These elements don’t cause eyelid eczema directly, but they do make a flare-up worse, harder to heal, and more likely to recur.
- Stress and Fatigue: A 2020 survey found that 57% of women and 41% of men reported stress worsened their symptoms. Emotional pressure causes your body to release inflammatory chemicals, slowing down the skin’s ability to repair itself.
- Poor Sleep and Alcohol: An increase in systemic inflammation throughout the body, such as that caused by poor sleep and alcohol, provides the perfect internal conditions for a susceptible area like the eyelids to react.
- Skin Dehydration: Central heating, cold air, or dry climate strip your skin of moisture. This physical dehydration compromises the barrier and exacerbates itchy eyelids.
Symptoms of Face & Eyelid Eczema
If you’re seeing a rough dry patch over your eyelids or dealing with relentless itchiness, it’s time to confirm your diagnosis. Here are the specific symptoms of eyelid eczema, broken down by stage.
Early Signs
Preventing a severe flare-up starts by recognising these subtle first symptoms. They’re the physical clues that your skin barrier is compromised and an inflammatory reaction is beginning.
- The First Warning: The onset of intense itchiness and a prickly tingling sensation. This is your skin’s heightened nerve response starting the scratch-itch cycle.
- Textural Change: The skin starts to feel dry, tight, and rough to the touch. This quickly manifests as a flaky texture or a tightening sensation, often triggered by washing your face.
Moderate to Severe Symptoms
The next stage is when a flare-up progresses past a simple itch, becoming more noticeable and painful.
- Persistent Inflammation: The eyelids will show persistent redness and become visibly swollen. This is the deep inflammatory reaction becoming entrenched beneath the thin skin.
- Cracking and Peeling: The prolonged dryness and inflammation cause the skin to crack, peel, or feel rough like sandpaper.
- Signs of Infection: In severe cases, you may see crusting, weeping, or a yellow discharge. This can indicate a secondary infection and requires prompt medical attention.
How It May Look on Different Skin Tones
Face and Eyelid eczema doesn’t always appear red. Presentation varies significantly depending on skin tone.
- Pale Skin: Typically shows as visible red or pink patches, accompanied by swelling and inflammation.
- Darker Skin Tones: Inflammation often causes the skin to appear brown, grey, or purple in colour. This hyperpigmentation becomes more pronounced with persistent flares.
- Universal Swelling: Regardless of skin colour, visible puffiness or swelling of the eyelids is a key sign that the underlying inflammatory reaction is well underway.
What’s the Difference Between Eyelid Eczema and Eyelid Dermatitis?
For most people, the terms eyelid eczema and eyelid dermatitis are used to describe the same symptoms of red, flaking, and itchy eyelids. However, understanding the subtle clinical difference helps pinpoint your cause.
What is Eyelid Dermatitis?
This is the broader term for any inflammation of the eyelid skin. Clinicians often use this term when the condition is caused primarily by an identifiable external irritant or allergen (Contact Dermatitis), such as a new cosmetic or airborne pollen.
In a 2024 referral study, the majority of cases, over 60%, were diagnosed as Allergic Contact Dermatitis, confirming that external product triggers are the single biggest cause of flares in the eyelid area.
What is Eyelid Eczema?
This term is often used more specifically when inflammation is linked to a chronic, genetic predisposition (Atopic Dermatitis). This type is tied to a faulty internal skin barrier and a personal or family history of related conditions like hay fever or asthma.
A major 2024 meta-analysis confirmed that Atopic Eczema is highly prevalent, representing 27.5% of all eyelid inflammation cases, underscoring the strong role of genetics.
The Takeaway: While the symptoms are the same, eyelid dermatitis highlights the trigger, and eyelid eczema highlights the chronic condition. Both require gentle care and active trigger avoidance.
How to Identify Your Triggers
Identifying the source of your eyelid eczema can feel like detective work. But it’s the most critical step to achieving lasting relief. Here are the most effective methods for tracking down your triggers.
- Start a Symptom Diary: Log your flare-ups, symptoms, and potential exposures (new products, stress, or seasonal changes). This often reveals patterns you wouldn’t notice otherwise.
- Use the Elimination Method: If you suspect a product, remove it completely for two weeks. Reintroduce one product at a time to isolate the culprit.
- Consider Patch Testing: For chronic or severe inflammation, consult a dermatologist for formal patch testing. This is the definitive way to diagnose a specific eyelid allergy.
- Track Lifestyle & Seasonal Patterns: Note if flares coincide with high-stress periods, poor sleep, or environmental shifts (like the start of hay fever season).
Need help knowing which ingredients to eliminate? Consult our detailed guide: Ingredients to Use and Avoid Near the Eyes.
When to Seek Professional Advice
While managing your eyelid eczema at home is the goal, you should never hesitate to reach out for help when things get worse. Consult a doctor or dermatologist if you see no improvement within 5-7 days of careful trigger avoidance and using gentle creams. Also, get immediate medical advice if you see any signs of infection, such as intense pain, severe crusting, or yellow/green pus, or if the inflammation is causing vision problems.
Your Eyelid Eczema Management Starts Now
Stop treating your eyelids like any other part of your body! They are hyper-reactive and deserve special, gentle care. Relief from eye eczema comes with diligence: identifying and eliminating those sneaky triggers and consistently supporting the thin skin barrier.
Ready to find relief? Discover Dermal Therapy Face & Eyelid Eczema Cream, specifically formulated with 5% Colloidal Oatmeal to soothe irritation and provide steroid-free relief from eye eczema.
Learn more in our relevant articles:
- Eyelid Eczema: Causes and Symptoms
- How to Manage & Treat Eczema Around the Eyes Safely
- The Role of Emollients in Eczema Management
- What Could Be Causing Your Facial Eczema and Irritated Skin
- Understanding Eczema in Babies and Children: Tips for Parents
- Eczema and Mental Health
References:
- Scielo Brazil: Demographic and clinical characteristics of patients with eyelid eczema
- Pubmed: Eyelid dermatitis in patch-tested adult patients
- Eczema.org: Eczema Unmasked
- Wiley Online Library: The Impact of PPD-related allergic contact dermatitis
- Pubmed: Eyelid dermatitis in patch-tested adult patients